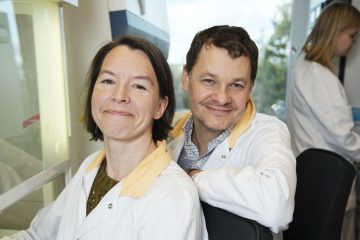
STUDY. Researchers at Sahlgrenska Academy and Sahlgrenska University Hospital have mapped the genome of metastases from uveal melanoma, a rare but severe form of malignant melanoma that originates in the eye. The knowledge provided by this gene mapping includes new insights into how metastases arise and the nature of tumor-infiltrating immune cells.
The study, now published in Nature Communications, provides hope for new approaches to combating this form of tumor.
Control of gene expression connected with prognosis
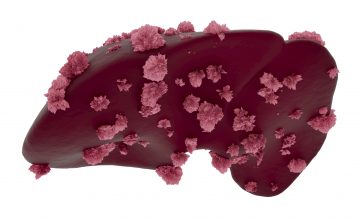
Malignant melanoma is a form of cancer that develops in natural pigment (melanin) cells — usually in the skin, but there is also a more unusual form that starts in the eye. This ocular form, known as “uveal melanoma”, affects some 80 people a year in Sweden. It is often treated with radiation or, in some cases, surgical removal of the eye, both of which cures approximately half of the patients.

“Interestingly, the prognosis coincides with how the genes are ‘read’ — that is, the reading of the genes in the tumor’s genome. If the patient’s tumor has a particular gene ‘signature’ (or ‘profile’), metastases never arise, strictly speaking. If the tumor has a different gene signature, on the other hand, metastases develop, above all in the liver; and the disease is then incurable,” says Jonas Nilsson, Professor of Experimental Cancer Surgery at Sahlgrenska Academy.
First sequencing of metastases’ genome
Several major studies have previously mapped (or “sequenced”) the genome of ocular melanoma, one outcome being a diagnostic test based on the gene signature. However, these studies have focused on tumors that have developed in the eye, not tumors that have grown as metastases in the liver, for example. One reason why the genome of these metastases has not been sequenced on such a large scale is that tumor samples are seldom taken in patients with uveal melanoma when they develop metastases. As a result, no biobank of high-quality material for sequencing has been available world-wide.
Study enabled necessary biopsies
For the past few years, a clinical trial known as the SCANDIUM study, for patients with liver metastases from uveal melanoma, has been underway in Gothenburg.

“We connect the liver to a heart–lung machine and wash the liver with extremely high doses of cytostatic drugs — a treatment called ‘hepatic perfusion.’ We’ve known for some time that patients have responded to this treatment, but we don’t yet know whether the treatment can prolong survival for this category of patients. We’re therefore carrying out a randomized study in which half of the patients get isolated hepatic perfusion and the other half get another form of systemic treatment,” says Roger Olofsson Bagge, a surgeon at Sahlgrenska University Hospital and Associate Professor (docent) at Sahlgrenska Academy.
In conjunction with this treatment, the surgeon was often able to cut away superficial biopsies of metastases in the liver. These biopsies were immediately dispatched to the laboratory, and Professor Nilsson relates that having access to such fresh tumor samples has been highly advantageous.
“We were able to save one piece for analysis of its genome and RNA, and another for culturing the immune cells found in the tumor. Another piece of the biopsy was used in the animal model known as ‘patient-derived xenograft’ (PDX) mice, where mice become carriers of human tumors and, that way, like avatars for the patient’s tumor disease.”
Identifying genetic change
The study shows that the majority of mutations, 90 percent, had mutations in the BAP1 gene. A couple of the metastases had also lost the CDKN2A melanoma gene. Changes in certain major chromosome segments proved to be more common than it had previously been possible to see in eye tumors. Some of the mutations in the BAP1 gene require investigation also of regions that do not directly code for protein.
“Since BAP1 mutations proved to be much more common in uveal melanoma than we’d previously thought, we wanted to investigate which function this gene has in the tumor cells,” Nilsson says.
Gene signature connected with prognosis
Tumor cells that had first been allowed to grow in a PDX mouse, created by researcher Lisa Nilsson, proved capable of subsequently growing in a cell culture incubator. She used a virus to insert a correct form of BAP1 in the cell, which thus suddenly regained the BAP1 protein. When the research team then compared gene expression in the cells that lacked BAP1 with that of the ones in which BAP1 had been restored, they noted something extremely surprising.

“It turned out that much of the gene signature that can distinguish uveal melanomas with a poor prognosis from the ones with a good prognosis may in fact be regulated by BAP1,” Joakim Karlsson says.
Damage from UV light
Another surprising finding was that the genetic material from one of the tumors appeared to be damaged by ultraviolet (UV) light, exactly like skin melanoma. Exposure to sunlight is not usually considered to be a risk factor for uveal melanoma, at variance with it being the major risk factor for skin melanoma. Interestingly though, the tumor with UV damaged DNA turned out to have arisen in the iris, which is located in an superficial position in the eye and could therefore very well have been exposed to solar UV radiation. Iris melanoma is highly unusual, being only 1 percent of all uveal melanomas, which explains why the connection between iris melanoma and exposure to UV light has not been found earlier. The research group gained access to samples from another patient with iris melanoma, who also showed signs of UV damage to the genome.
Cross-fertilizing studies
The study also presents interesting findings about the immune cells known as tumor-infiltrating lymphocytes. Sequencing of individual cells enabled study of both gene expression and receptors in the T cells. Different patients’ uveal melanoma metastases proved to have varying sets of T cells that partly expressed genes other than those that are common among the T cells that infiltrate skin melanoma. This may be a partial explanation of why uveal melanoma is more difficult to treat with immunotherapy than skin melanoma.
The research group is currently analyzing the results of another clinical study (the PEMDAC study), coordinated by oncologist Lars Ny. This study uses a combination treatment in which a drug that alter gene expression (HDAC inhibitor) is combined with an immune checkpoint immunotherapy (PD-1 inhibitor). This hope is that the combination will be able to cause uveal melanoma tumor shrinkage just like single PD-1 inhibitor can do in skin melanoma but cannot do in uveal melanoma.
“The study that we’ve now been able to publish in Nature Communications has contributed valuable knowledge in real-time for the two ongoing studies SCANDIUM and PEMDAC, and in all likelihood will influence future studies concerning patients with metastasized eye melanoma,” Jonas Nilsson says.
The task of analyzing the genome in this study was performed first by SciLifeLab in Stockholm and subsequently by Genomic Center West (GMC West), part of Genomic Medicine Sweden (GMS). The bioinformatics work was carried out by first author Joakim Karlsson, a former PhD student in Erik Lekholm’s group, who is now a postdoctoral researcher in Jonas Nilsson’s group.
Read the study in Nature Communications here: https://rdcu.be/b3Fr0
TEXT: ELIN LINDSTRÖM











